Latest NUCDF News
In February 2025, the parents of KJ Muldoon agreed to let doctors treat their son with a new experimental therapy. Their decision opened the door to one of the most talked-about medical breakthroughs of the year. While the revolutionary treatment helped only one baby, it broadly raised hopes among the UCD patient community. How can more patients benefit from this advance?
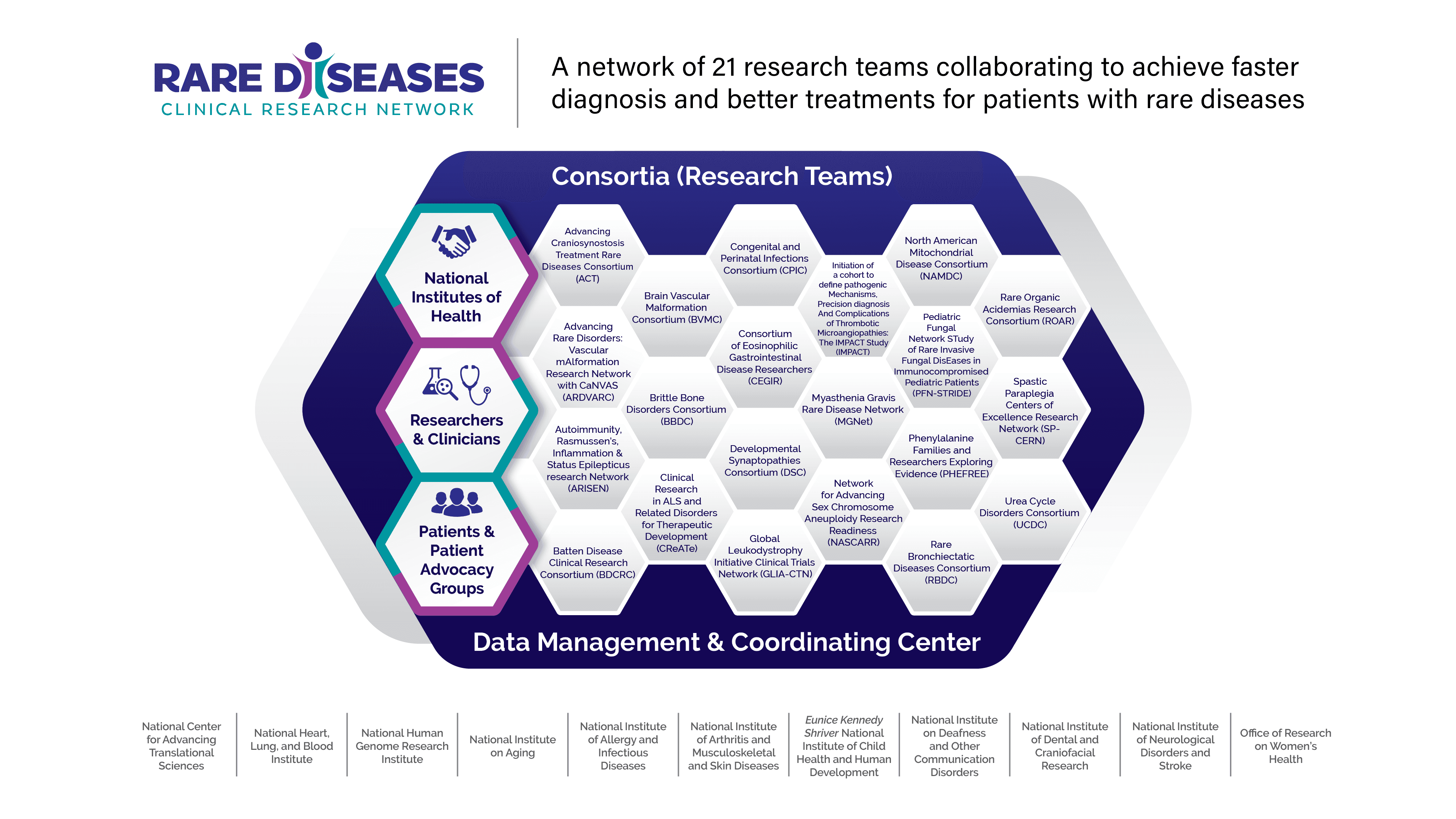
The Urea Cycle Disorders Consortium (UCDC), NUCDF's research partner, was recently awarded a no-cost extension to continue its participation in the NIH's Rare Diseases Clinical Research Network (RDCRN). The UCDC, which has been continuously funded under the RDCRN program since 2003, is among the 21 leading rare disease research teams included in the network's fifth funding cycle.
At the National Urea Cycle Disorders Foundation (NUCDF), our mission has always been to connect, support, and advocate for families affected by Urea Cycle Disorders. Today, we are sharing an important update from our partners at the National Organization for Rare Disorders (NORD) regarding their UCD Patient Assistance Program.
NUCDF recognizes that there is uncertainty regarding generic glycerol phenylbutyrate. We have heard the concerns expressed by the patient community regarding the timing and availability of generic options and what impact that may have on patient access to these lifesaving medications.
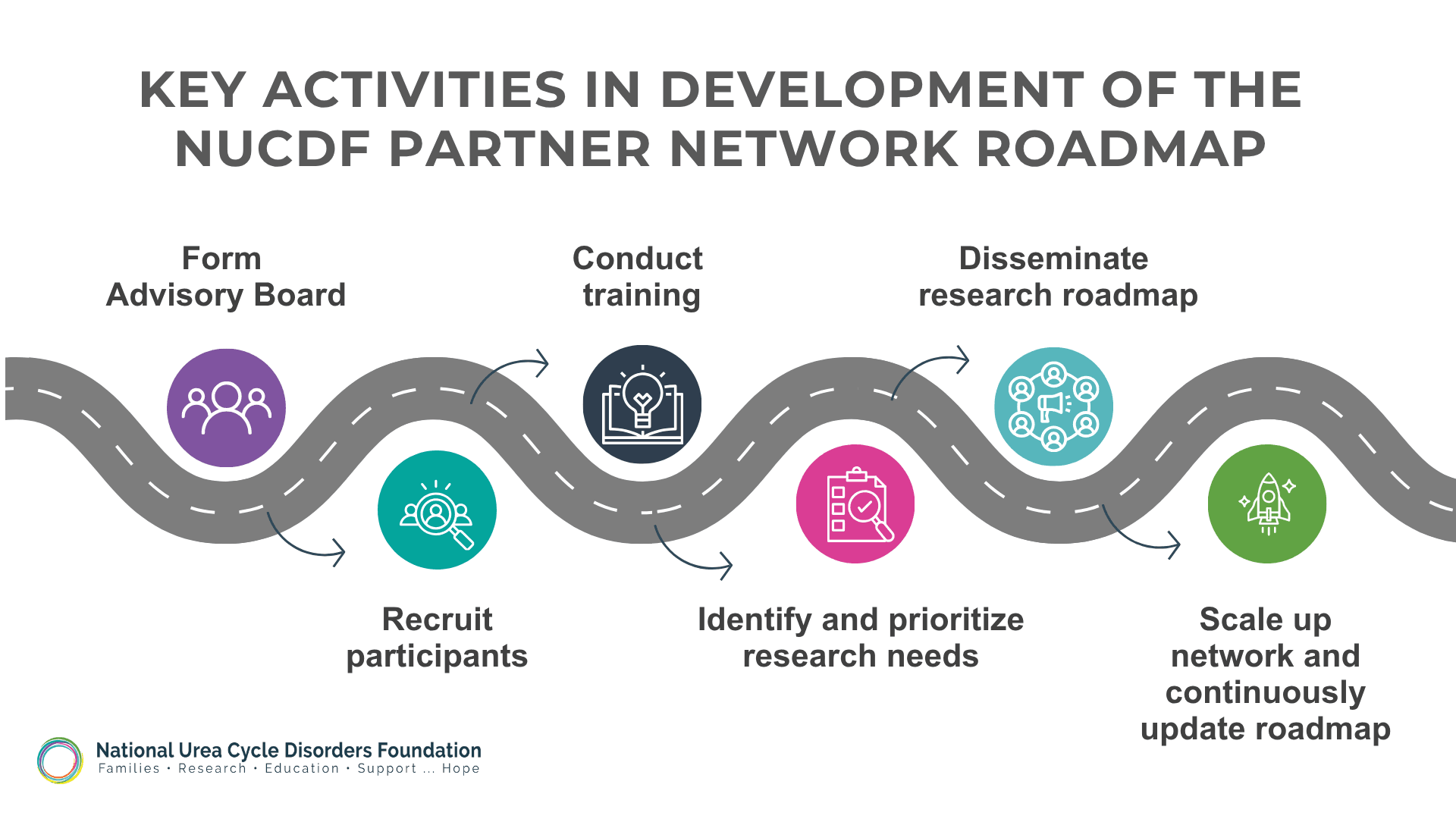
Patients and caregivers affected by urea cycle disorders (UCDs) can now apply to join the NUCDF Partner Network, a new initiative that offers more stakeholders a greater voice in planning the UCD research agenda.
October is Check Ammonia Month, an annual campaign to improve the diagnosis of urea cycle disorders (UCDs) by highlighting the critical importance of promptly checking blood ammonia levels and using proper testing techniques. Patients, providers, and the public are invited to help save lives by sharing messages and materials from CheckAmmonia.com.
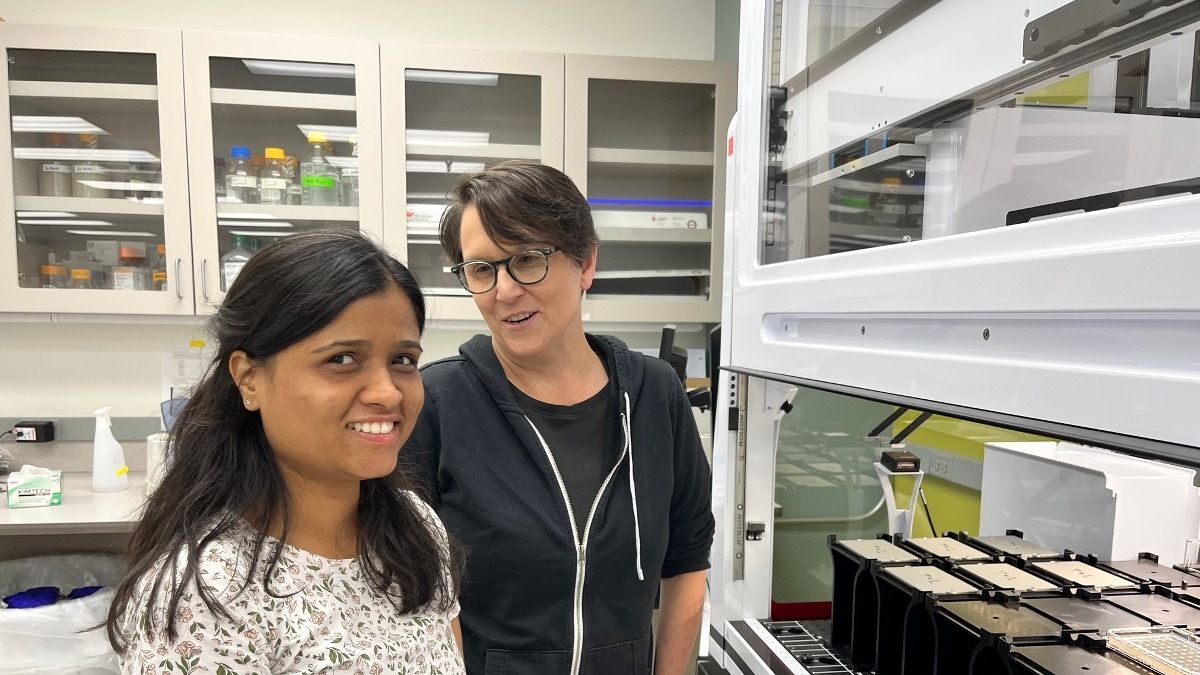
NUCDF has awarded the 2025 Cynthia Le Mons Fellowship to Shradha Suyal, PhD, a postdoctoral fellow at the Pacific Northwest Research Institute (PNRI), for research in arginase-1 deficiency. The fellowship is funded by NUCDF’s annual Cure the Cycle event. This year, the Arginase 1 Deficiency Foundation is also lending support.
The state of Florida is investing more than $7 million to pay for whole genome sequencing for newborns under the Sunshine Genetics Act, which took effect July 1, 2025. The law establishes a five-year genetic testing pilot program for newborns.
The National Urea Cycle Disorders Foundation (NUCDF), the leading patient advocacy group for people affected by urea cycle disorders (UCDs), today announced the launch of a two-year national project to establish the multistakeholder NUCDF Partner Network and develop a roadmap for future research in these rare disorders.
The first session of NUCDF's new educational series for clinicians, "Urea Cycle Disorders ECHO: The Essentials," featured Lindsay Burrage, MD, PhD and focused on recognition and testing of these rare genetic metabolic disorders.
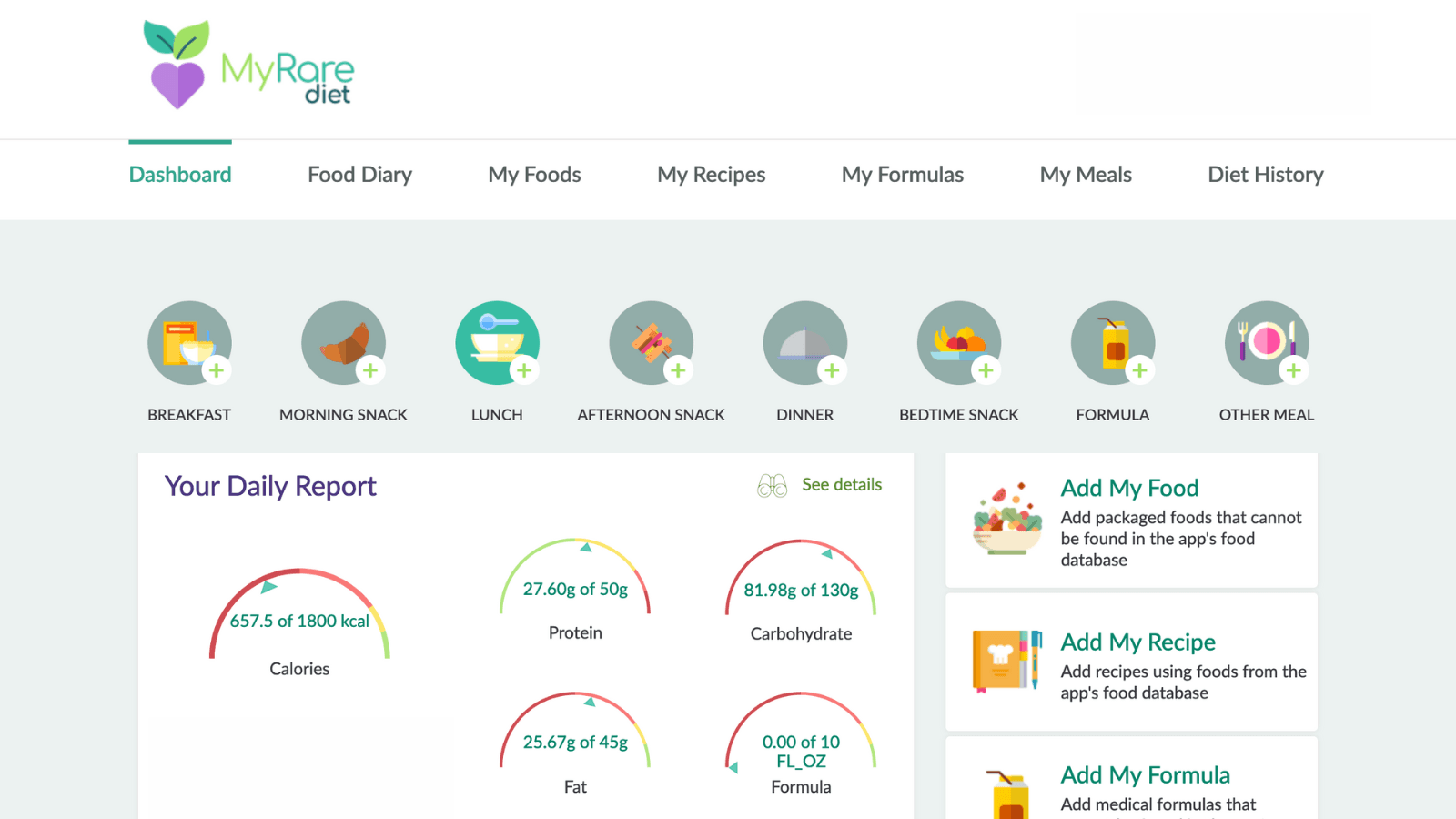
MyRareDiet is a nutrition software application and mobile health tool currently being tested that can be used in research, clinical trials and patient dietary management
A new report published by the National Academies of Science, Engineering and Medicine on May 1 issued actionable recommendations designed to preserve and enhance this critical public health program.
The National Urea Cycle Disorders Foundation (NUCDF) is launching a new educational series for clinicians, “Urea Cycle Disorders ECHO: The Essentials,” in partnership with Project ECHO. Four educational sessions will be offered in 2025 focusing on recognition, diagnosis, and treatment of urea cycle disorders (UCDs).
New research examines risks, outcomes of seizure activity in patients with inborn errors of metabolism hospitalized with high ammonia and recommends more neuromonitoring
PRESS RELEASE: NUCDF and Zevra Therapeutics, Inc. are teaming up to launch an awareness campaign during the month of October to improve the diagnosis of urea cycle disorders (UCDs)
Exploring Sibling Dynamics: The Blessings and Challenges of Having a Sibling with a UCD
Several recent papers on citrin deficiency are offering new insights into the disease, its prevalence, and currently available treatment options.
A July tornado in Mount Vernon, Indiana is threatening supplies of Reckitt/Mead Johnson metabolic formulas
Kids with urea cycle disorders (UCDs) need special attention to manage their condition effectively.
An NUCDF grant to the Pacific Northwest Research supported the purchase of equipment for ongoing research into the significance of urea cycle disorder (UCD) variants.
New research shows that female OTC carriers face both symptoms and health risks at higher levels than previously thought. Study authors say they should be monitored to reduce risks and possibly treated.
A new therapy that offers dramatic improvement for patients with the condition has been approved for use in Europe and is currently following the process for approval in the U.S.
While the physical manifestations of UCDs are well-documented, their impact on mental health is also an important factor.
In early April, the 2024 NUCDF Family Conference “Legacy of Hope” welcomed 54 families from the U.S., Puerto Rico, Brazil, Peru, El Salvador, and Canada, as well as nearly 40 medical professionals.
Since its founding in 1988, NUCDF has relied on a core team of medical professionals with expertise in research and the many clinical care specialties related to urea cycle disorders.
Getting kids to take medicines can be a challenging task. Here are some strategies that may help make the process easier.
For families with children diagnosed with urea cycle disorders, life becomes a delicate balance of medical management, emotional resilience, and unwavering support.
By exploiting the technology used in Covid-19 vaccines, a team has created an effective therapy for arginosuccinic aciduria in a study in mice, demonstrating the technology’s potential therapeutic use in people.
A research team exploring the inheritance patterns of late-onset ornithine transcarbamylase deficiency (OTCD) has described two families showing father-to-daughter transmission of the disorder.
A research team has developed a method using yeast genetics to rapidly measure the effects of thousands of variants of a gene that causes human disease, with the aim of improving diagnosis of urea cycle disorders.
Experts from the Urea Cycle Disorders Consortium and the National Urea Cycle Disorders Foundation share what they're learning from the “Longitudinal Study of Urea Cycle Disorders.”
New research finds that the nitric oxide deficiencies common in arginosuccinate lyase deficiency (ASLD) create problems with the blood brain barrier, which is essential to maintaining brain health.
New research explores faster and more accurate diagnosis of urea cycle disorders (UCD), variants of uncertain significance, life with a UCD, and more.
Washington, D.C. – Following unanimous support in the Texas House of Representatives and a 30-1 vote in the Senate, Texas Governor Abbott affirmed the state's status as a leader in newborn screening by signing House Bill 2478 into law.
Five months after his death, Robbie Roper's family reveals that his tragic passing was caused by an undiagnosed urea cycle disorder. Robbie received corticosteroids - a known trigger for hyperammonemia - during shoulder surgery, leading to fatal hyperammonemia.
NUCDF and the Urea Cycle Disorders Consortium (UCDC) partner to advance research. Read more about the partnership and current research studies.
NUCDF and the Rare Diseases Clinical Research Network Urea Cycle Disorders Consortium (UCDC)co-host the 5th International Scientific Symposium on Urea Cycle Disorders, "Mapping Progress: Current Concepts and New Insights in Urea Cycle Disorders," on September 22-24, 2021. Read more.
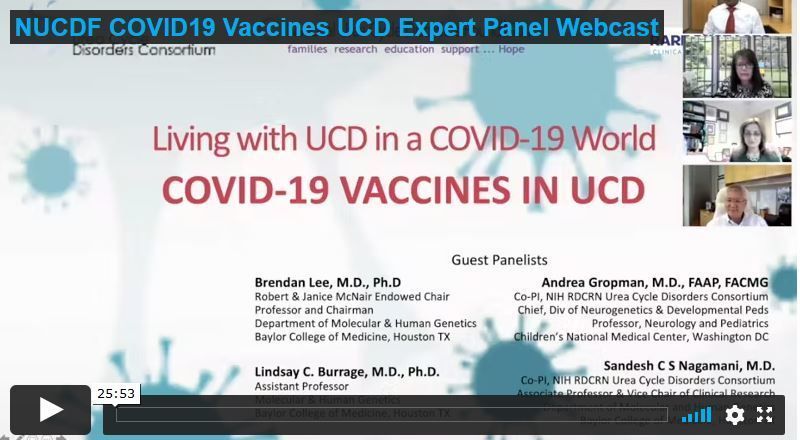
UCD experts, Brendan Lee M.D. Ph.D., Sandesh Nagamani M.D., and Andrea Gropman M.D., provide general guidance about COVID-19 vaccines in individuals with UCD and answer questions submitted by our UCD community. Presented in partnership by NUCDF and the NIH Rare Diseases Clinical Research Network Urea Cycle Disorders Consortium (UCDC).
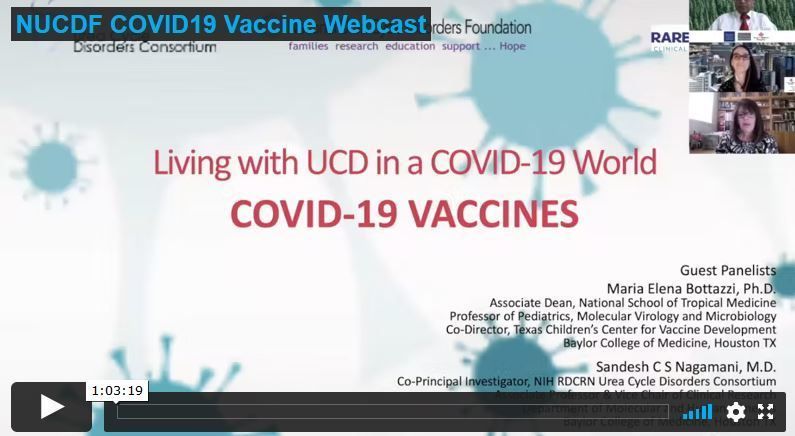
Dr. Maria Elena Bottazzi, internationally-recognized vaccinologist, provides information and answers questions from our UCD community about the development and types of current vaccines, safety and effectiveness. Presented in partnership by NUCDF and the NIH Rare Diseases Clinical Research Network Urea Cycle Disorders Consortium (UCDC).
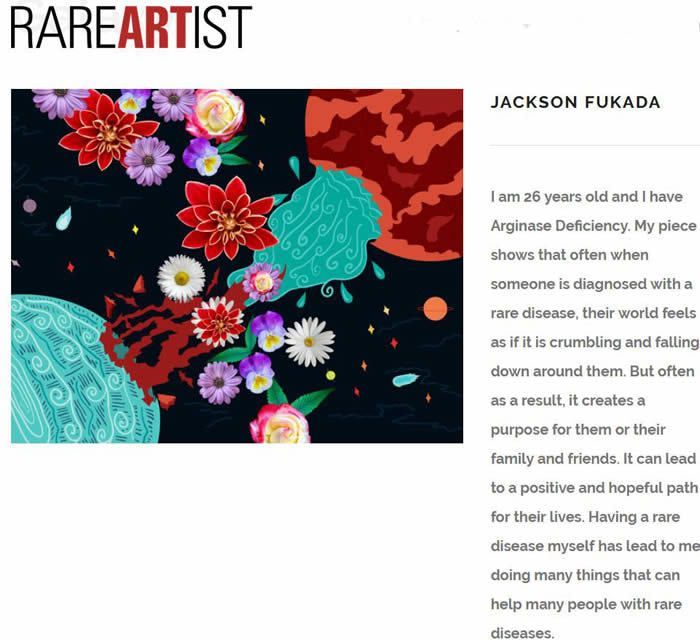
UCD warrior Jackson Fukuda has won the Rare Artist Award as part of Rare Disease Day
Raising awareness of UCDs on Rare Disease Day
Swift identification of elevated ammonia levels in the ER is needed to save lives. An affected family has partnered with NUCDF to raise awareness and educate medical professionals on the need to obtain blood ammonia levels.
Body builder Meegan Hefford has died from hyperammonemia from undiagnosed OTC deficiency.
The long-awaited clinical trial "Effect of Nitric Oxide Supplementation on Neurocognitive Functions in Patients With Argininosuccinate Lyase Deficiency/Argininosuccinic Aciduria (ASLD/ASA)" is now open for enrollment at Baylor College of Medicine (one of the UCD Research Consortium clinical research sites) in Houston, Texas.
A young college student has died from undiagnosed OTC deficiency.
Pharmaceutical industry sponsored clinical trial recruiting participants to test safety and effectiveness of enzyme replacement therapy for Arginase Deficiency.
NUCDF funds two new UCD clinical research sites at Stanford/Lucile Packard Children's and University of California San Francisco.